The transition from pediatric to adult healthcare and services is an essential event in the life course of all youth, including youth living with medical complexity. Data from the National Survey of Children’s Health indicates that less than 20% of youth receive support for healthcare transition (HCT). Medical and technological advances have significantly increased the life expectancy of children and young adults living with medical complexity (YAMC), so this population is transitioning from pediatric to adult care systems more than ever before.
HCT matters because a successful transition means YAMC can continue their care without a gap, reducing the need for emergent and unplanned care that can impact overall health. Yet barriers to successful HCT for YAMC persist.
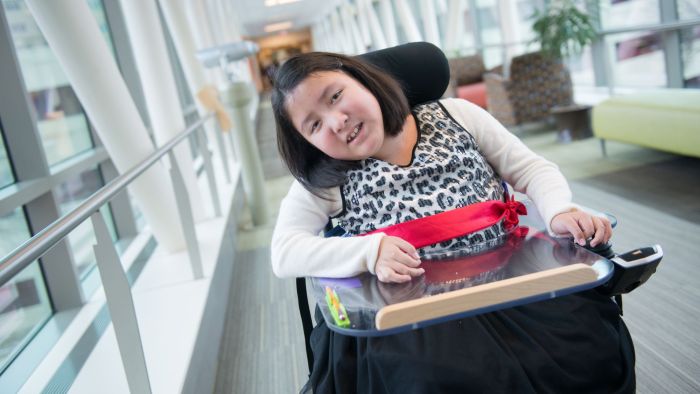
To understand the support, tools, and resources that facilitate successful HCT for this population, Gillette Children’s recruited three groups of participants to share their lived experiences of "what worked" and "what is needed" for successful healthcare transition.
The Focus Group
Group #1: Young adults aged 24-32 who are their own legal decision-makers and living with cerebral palsy, spina bifida, or muscular dystrophy
Group #2: Parents of young adults in Group #1
Group #3: Parents of young adults aged 24-32 who are not their own legal decision-makers and living with cerebral palsy, spina bifida, or muscular dystrophy
The Takeaways
The voices of 10 young adults and 14 parents emerged in three key takeaways under an overarching theme: HCT is an individualized process with success relying on consistent, clearly defined, and system-wide guidelines and resources.
Key Takeaway 1
The lack of system-level capacity (healthcare, insurance, home nursing) resulted in losing resources and support when the individuals moved from pediatric to adult systems. All participants agreed that successful HCT is often guided by individual clinicians and overwhelmingly expressed appreciation for these individuals. However, moving from pediatric/family-centered health systems to adult/patient-centered health systems requires increased self-management, and young adults often felt under-prepared for this role.
Key Takeaway 2
Moving into adulthood is multifaceted and involves changes in healthcare providers and systems, as well as decisions on education, employment, vocational rehabilitation, and where a young adult will live. These transitions occur in different systems, on different timelines, and are often limited by laws on communication and information sharing. Support from formal transition coordinators would improve communication between the multiple health, county/state agencies, and education systems involved during this period.
Key Takeaway 3
Formal peer support programs are needed for young adults with medical complexity and their parents. While participants appreciated Gillette-sponsored social media groups for sharing information and resources, they all agreed that virtual or in-person support groups could provide greater socioemotional and logistical benefits.
Taken together, these findings should serve as a foundation for organizational and system-level capacity that supports the successful transition of all youth from pediatric to adult care systems.
*Wilder Research facilitated all focus group sessions and subsequent content analysis to ensure participants felt safe expressing viewpoints that could be viewed as critical of Gillette services.
Join Our Partners in Care Community!
Subscribe to Partners in Care Journal, a newsletter for medical professionals.
Subscribe Today Home Page
Home Page