The focus of research at the Gillette Spine Institute is investigating neuromuscular scoliosis (i.e., lateral curvature of the spinal column in patients with neurologic conditions). For these patients, spinal curvatures can have significant effects on health, comfort, skin integrity, and quality of life.
Spinal fusion surgery is typically performed for patients with severe curvatures in hopes of improving or maintaining lung function, seating comfort, and health-related quality of life. Currently, “success” of spinal fusion surgery is often based on radiographic markers of spinal curvature and balance even though the clinical significance of these variables with respect to seating, comfort, and skin integrity is poorly understood.
Seating Pressures in Neuromuscular Scoliosis
The Seating Pressures in Neuromuscular Scoliosis pilot study is led by principal investigator Dan Miller, MD, and supported by spine researchers Sara Morgan, PhD, and Zelphia Brown, MPH, and members of the Gillette Children’s orthotics, prosthetics and seating team, including Nick Anderson, DC, ATP, and Joe Berdan, ATP.
Supported by the Pediatric Orthopaedic Society of North America (POSNA) St. Giles Young Investigator Award, the study is investigating the effects of spinal fusion surgery on measures of seating pressures, and patient-reported seating comfort in non-ambulatory children with neuromuscular scoliosis associated with cerebral palsy.
To achieve these objectives, non-ambulatory patients aged 10 to 21 years with neuromuscular scoliosis undergoing spinal fusion surgery are evaluated before and after surgery. These evaluations are intended to assess if spinal fusion surgery changes the way people with neuromuscular scoliosis sit in a wheelchair, including the amount of pressure on the skin and their overall sitting comfort.
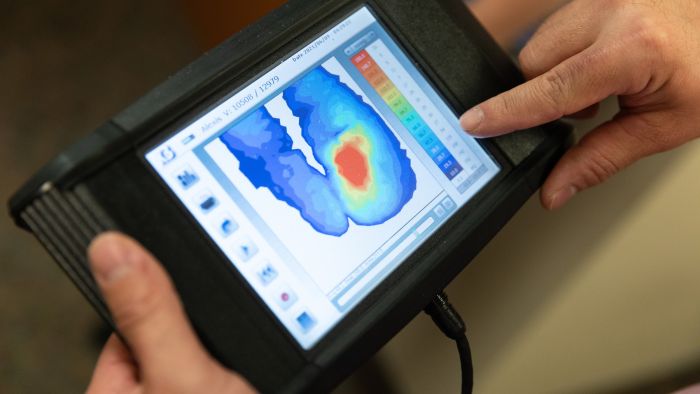
During these evaluations, the study team utilizes an Xsensor pressure mapping mat. The pressure mapping system gathers detailed information about the average, peak, and minimum pressure experienced by participants as they sit on a flat surface. By integrating this quantitative data with radiographic imaging and patient reported outcomes surveys from the participants’ parents, the research team gains a more comprehensive understanding of the seating impacts of spinal fusion surgery.
Patient-Reported Outcomes Are Key
Dr. Morgan believes patient-reported outcomes are integral to the pilot study, providing valuable insight into the patients’ experiences. She says, “We’re focused on the outcomes and treatments that matter most to patients. We work to engage patients with spinal conditions and their families in our research program to ensure that our research is meaningful in the lives of the patients that we treat.”
Results from this line of research will facilitate preoperative counseling and shared decision-making with patients and their caregivers, as well as possibly improve elements of patient care before and after spine surgery. This data will be relevant not only to pediatric patients with neuromuscular scoliosis, but also to patients with spinal cord injury and adult patients with other neuromuscular conditions and spinal deformities.
Enrollment in the study is underway, and the team anticipates enrolling a total of 30 participants. With a two-year follow-up period, the Seating Pressures study is expected to conclude in 2026.
Get Partners in Care Stories in your inbox!
Subscribe to Partners in Care Journal, a newsletter for healthcare providers and community health professionals.
Subscribe Today Home Page
Home Page