What is spondylolysis?
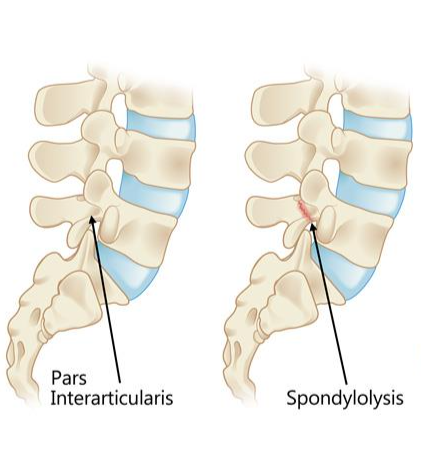
Spondylolysis describes a stress fracture through the pars interarticularis (the thin bones that connect two vertebrae in the spine).
The pars interarticularis is a thin bone between two joints. It can be a weak area of the spine and therefore is an area that may be more likely to be injured by repetitive stress or a back bending motion. Spondylolysis is fairly common; approximately 5-6% of kids and teens have had spondylolysis by the time they are 18 years old.
What are the symptoms of spondylolysis?
Most people have no symptoms with spondylolysis. For those that do, the most common symptom is back pain. The body treats this injury like a broken bone and responds with inflammation and discomfort. The inflammation can cause back pain, hamstring tightness, and soreness when standing or walking. The pain is usually in the lower back (lumbar) region and is made worse with activity and sports.
Spondylolysis is typically associated with activities that require repetitive arching or bending of the back (extension) such as gymnastics, volleyball or tennis serves, or offensive lineman play.
What are the risk factors for spondylolysis?
Walking upright is the basic risk factor for spondylolysis. The natural sway and curve of the low back puts stress on the pars interarticularis. Sports and activities that have repetitive extension of the lower back increase this stress and can put someone at a higher risk. As mentioned above, common sports that can lead to spondylolysis include gymnastics, dance, football, tennis, weight lifting, and volleyball. Genetics could be a risk factor, but there is no definitive proof of that at this time.
How is spondylolysis diagnosed?
Since it is possible to have spondylolysis and not have any pain or symptoms, sometimes spondylolysis is identified on imaging that was done for another purpose (a scoliosis screening, for example). This is called an incidental finding.
Persistent and/or worsening of lower back pain is a reason to be seen by a healthcare provider. An x-ray is the first step in identifying a pars stress fracture. However, sometimes we are unable to see the defect on an x-ray. If the physical exam and history of pain are consistent with a spondylolysis, treatment may be an option. Some patients may have an MRIor CT scan performed to help confirm the diagnosis.
What is the treatment for spondylolysis?
If there is no pain, no treatment is needed. There are no restrictions or extra precautions that need to be taken. This does not put the spine or spinal cord at higher risk of injury. Spondylolysis is NOT a dangerous condition.
For someone experiencing symptoms, treatment focuses on managing pain, with a goal of returning to daily activities and a full return to athletics. At Gillette, we use a step-by-step approach to manage pain and safely and gradually return to activities. This is the best way to prevent repeat injury and pain.
| Stage | Rest/Protection | Rehabilitation Foundation | Rehabilitation Recovery | Rehabilitation Function | Return to sport |
| Exercise phase | 1 | 2 | 3 | 4 | 5 |
| Focus | Rest/protection, core initiation, abdominal bracing | Isometric stabilization | Dynamic stabilization and coordination | Athletic enhancement, slow return to activity | Maintenance exercise routine |
| Duration | 4-8 weeks | +1-4 weeks | +2-4 weeks | +2-6 weeks | Total 3-6 months |
Duration: 4-8 weeks, depending on your progress. To ensure proper healing of the spondylolysis, it is important to rest completely and for the entire length of time recommended by your spine provider. A course of anti-inflammatory medication (a prescription steroid course, or over-the-counter ibuprofen or naproxen) may be recommended by your provider. Bracing is a very commonly implemented treatment utilized to not only potentially speed the rate of pain relief, but also to immobilize the spine and protect the spondylolysis from further irritation/activity.
Rehabilitation Goals
- Allow sufficient time for healing to occur.
- Pain-free with daily activities
- Gradually increase flexibility of key upper and lower body muscles.
Restrictions and Precautions
- Bracing as instructed by spine provider.
- No sports or activities (including gym class).
Suggested Therapeutic Exercises
- No formal physical therapy yet.
- Abdominal bracing in various postures
- Stretching exercises for key muscles with emphasis on neutral spine alignment and in non-weight bearing postures.
Progression Criteria
- Pain-free activities of daily living
Follow Up
- 6 weeks from the first visit with spine provider may be recommended.
Duration: Additional 1-4 weeks to master foundational movement patterns.
- Start formal physical therapy (PT).
- Begins after the 4-8 weeks of necessary rest required to achieve significant pain reduction.
Rehabilitation Goals
- Maintain pain-free (or nearly pain-free) range of motion
- Pain-free with daily activities · Increased core strength
- Ensure normal hip and thoracic mobility
- Progress flexibility and lumbar stabilization to weight-bearing postures
- Improve pelvic alignment and balance
- Maintain/increase flexibility in key upper/lower body muscles
Restrictions & Precautions
- Bracing as instructed by spine provider
- No sports or activities (including gym class)
- No active or passive lumbar extension (back bending)
- No running or jumping
Suggested Therapeutic Exercises
- Formal physical therapy starts
- Isometric core exercises
- Continue stretching
- Non-impact aerobic fitness (elliptical, biking)
Progression Criteria
- Noticeable increase in abdominal strength
- Can accomplish full and pain-free lumbar flexion and lateral extension range of motion
- Ability to hold bridge side plank for 30 seconds without pain
- Ability to maintain neutral spine posture during dynamic arm or leg range of motion
Duration: Additional 1-4 weeks to achieve this phase. On average, this will phase will begin about 2 months from Day #0 (first day of true rest from activity).
- Continue formal physical therapy
Rehabilitation Goals
- Continue increase in abdominal strength.
- Maintain flexibility.
- Ensure normal joint mobility: hip and thoracic spine.
- Resume lumbar extension in non-weight bearing postures.
- Progress aerobic fitness.
Restrictions & Precautions
- Bracing as instructed by spine provider, probably wean from brace.
- No sports or activities.
- No sprinting, no jumping.
- No hyperextension of lumbar spine (No back-walk overs).
Suggested Therapeutic Exercises
- Continue physical therapy.
- OK to begin jogging.
- OK to resume upper body weight lifting with spine neutral.
Progression Criteria
- No increase in pain with lumbar range of motion and sports skills.
Follow Up
- 12 weeks from first visit with spine provider may be recommended.
Duration: 2-4 weeks to achieve the goals depending on the individual.
- Continue formal physical therapy.
- This phase takes into account the unique demands of the sport: progresses into impact loading through running and jumping, provide sport-specific exercises, and leads to the development of a maintenance program.
Rehabilitation Goals
- Maintain abdominal and hip muscle strength.
- Maintain flexibility in key muscle groups.
- Initiate lumbar extension AROM if necessary for sport.
- Initiate impact loading of the spine – jumping, landing, running.
Restrictions & Precautions
- Careful return to sport-specific activities with guidance from PT.
- The last movements to be attempted should be hyperextension of lumbar spine.
Suggested Therapeutic Exercises
- Progression to impact loading
- Bodyweight exercises
- Gradual exposure to sport-specific activities and drills, making sure to concentrate on spine stability.
Progression Criteria
- Successful completion of comprehensive exercise program.
- Be able to demonstrate sport-specific skills and practice drills without pain.
At this point, you are cleared to participate in your athletics. Your physical therapist will provide you with specific exercises that will aim to enhance your athletic performance and may help to prevent future injuries.
Rehabilitation Goals
- Full participation in sports
- Pain-free daily activities
- Commit to completing a 10-15 minute abdominal workout at least 3 times a week for the remainder of your athletic career.
Restrictions & Precautions
- May need to continue to avoid Olympic-style squats and deadlifts (powerlifting).
Suggested Therapeutic Exercises
- Personalized home maintenance exercise routine as discussed with a physical therapist.
Is surgery needed for spondylolysis?
In the majority of spondylolysis cases, no surgery is needed.
In rare cases, when pain is persistent despite rest and physical therapy, is adversely affecting daily life, is repeatedly painful, and/or all other potential causes of pain have been explored, surgical options can be discussed.
Spondylolysis Care at Gillette Children's
At Gillette, you’ll have access to a team of nationally recognized pediatric orthopedic specialists that understand how spondylolysis can affect health, self-esteem and quality of life. Our goal is to help your child achieve the highest levels of health, independence and happiness.
Your family will work closely with experts on a custom and comprehensive treatment plan that meets your needs. Specialties and services most often involved in caring for kids who have spondylolysis include:
- Orthotics.
- Radiology and imaging.
- Rehabilitation therapies, including physical therapy.
- Child life.
 Home Page
Home Page


