What is a congenital nevus?
A nevus is a well-defined malformation of the skin. Typically it is hyperpigmented (has extra color) and sometimes has dark hair. (More than one nevus is “nevi.”) The term "congenital" means the lesion is present at birth. Some nevi are not noticed at birth, but develop during infancy. These are often less than 1.5 cm in diameter and appear before 2 years of age. They are referred to as early onset nevi, and affect 6-20% of teenagers or adults. They are different than congenital nevi, and often fall into the category of birthmarks.
Congenital nevi are generally classified into three categories:
- Small (<1.5cm)
- Intermediate/median (1.5 -19.9cm)
- Large/giant congenital nevi (>20 cm)
Some sources further define “giant” nevi as those lesions that:
- Cover greater than 30% of the body surface
- Are head/neck lesions, which are larger than the patient’s palm,
- Lesions, on body parts other than the head/neck, that are twice the size of the palm
About 80 percent of children with giant nevi have or develop “satellite” lesions. These smaller nevi can be found anywhere on the body. Measurements defining small to giant nevi are estimated numbers that we use to describe adult lesions. They’re based on what we estimate the nevi size to become with maturity. We scale down the size when we refer to neonates/infants.
How often do congenital nevi occur?
Small nevi occur in 1% of all newborns (1 in 100). Large/giant nevi occur in 1 in 20,000 newborns. Giant nevi covering greater than 70% of the body’s surface area occur in 1 in 500,000 newborns.
Giant nevi lesions typically occur in a “bathing trunk” formation, and are accompanied by satellite lesions. Giant nevi can also have areas that appear “lumpy” or uneven. These areas are usually painless, benign (non-cancerous) tumors within the nevus. Doctors might do biopsies of them or observe them for changes.
What causes congenital nevus?
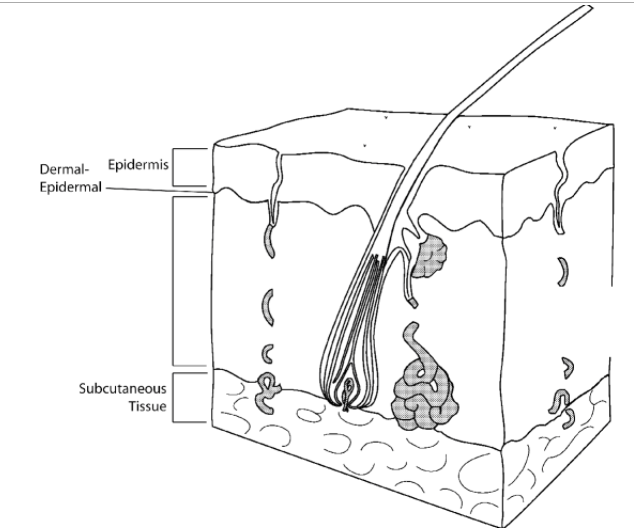
Congenital nevus has no specific cause. Nevi result from a localized overgrowth of melanin forming cells (the cells responsible for the pigmentation or color of skin). The diagram shows the different layers of skin. Nevi are classified by their appearance and location within these skin layers.
What are the most common types of congenital nevi?
- Compound nevi are nests of melanocytes (cells that produce skin coloration). They’re found in the epidermal-dermal junction and in the dermis.
- Halo nevus appears as a central brown mole surrounded by a uniformly depigmented (without coloration) area or “halo."
- Intradermal nevus is when melanocytes are found in the dermis, but not in the epidermal-dermal junction.
- Junctional nevus is categorized as melanocytes found in the basal cell zone, at the epidermal-dermal junction, and appear as a slightly raised, small, dark, and non-hairy lesion.
- Sebaceous nevus, an overgrowth in the epidermal layer of the skin, involves fatty glands. Often found on the scalp, these lesions are removed because they have the potential to become basal cell carcinoma in adulthood.
- Spitz nevi, sometimes called benign juvenile melanoma, are slightly pigmented or red lesions which can often be mistaken for worrisome melanomas in adults. For this reason, they are typically removed to avoid overly aggressive treatments later in life for this benign lesion.
When should congenital nevi be removed?
Surgical options for the removal of congenital nevi will be discussed when you consult with the surgeon. Individualized treatment plans are outlined based on each child’s need. Removal of small to medium- sized nevi is controversial, but some data suggests they can slightly increase the risk of skin cancer. For giant nevi, there’s increased incidence of serious melanomas later in life, so they should be removed.
How are congenital nevi removed?
Congenital nevi can be removed in one of the following ways:
Single excision: smaller nevi can be removed in one procedure. Typically, an elliptically shaped cut is made around the lesion. This allows the wound edges to come together in a straight line without any “puckered” edges. The length of the finished incision or scar will be approximately 3 times the transverse diameter (length) of the lesion. This is a same-day procedure.
Staged excision: nevi that are irregularly shaped or medium to large in size may require a staged procedure. The central aspect of the nevus is removed, using the same technique explained above. This incision is allowed to heal for 6-8 weeks. Then, another excision is made, removing more of the lesion. This is repeated until the lesion is completely removed. This is a same-day procedure that’s typically performed under general anesthesia.
Tissue expansion: for medium to large/giant nevi, tissue expansion may be indicated. Expanders also are frequently used for nevi located in the scalp/face/neck area. Expanders allow healthy surrounding skin to expand so that it can be placed over the area of the nevus after it is removed. This surrounding skin looks most like the skin near the reconstruction.
Usually, an incision is made within the nevus itself to insert the expander. The expander is placed under the skin, in the area of healthy tissue adjacent to the nevus. At the time of insertion, the expander may or may not be injected with normal saline to begin the expansion. If the area of expansion is too tight, the first injection may be deferred until the follow-up appointment. This procedure is performed under general anesthesia and requires an overnight stay.
Can congenital nevi grow back?
Congenital nevi typically do not grow back unless they aren’t completely excised. A margin of several millimeters is made outside the visible edge of the nevus. The tissue is sent to pathology for evaluation. Occasionally, the pathology results indicate that a few nevus cells were present in the margin of tissue and will be reported as an incomplete excision. Pathology reports are usually available by the time your child returns to clinic for a post-op check. If the report indicates incomplete excision, your surgeon will discuss with you whether more surgery is needed. Depending on the type of nevus, children might need follow-up appointments.
Will the congenital nevus be checked for malignancy?
Most nevi removed in children are benign. However, every time we remove a nevus of any type, we send it to pathology for examination. We report the results to you at the follow-up visit.
 Home Page
Home Page
